COVID-19: Persistent and Dangerous when Ignored
Infections, reinfections, and Long COVID remain under-recognised in workforce planning and public health policy.
COVID-19 has not disappeared. It continues to spread, disable, and disrupt lives - yet national strategies still appear to fail to acknowledge its persistence or the need for stronger infection prevention.
The mild… weather… has come to an abrupt end in the UK. Temperatures have dropped significantly - and there has been a period of significant rainfall over the past few days. Schools are back from their autumn half-term break, and after the busiest October on record for Accident and Emergency Departments of our already under pressure hospitals, the NHS is heading into a winter storm of pressures because of rising demand, resident doctor’s industrial action, and an early influenza season that many believe could be the worst in years.
Why does this absence matter? Because of the impact on patient health and wellbeing, and the impact on staff absence (not only in the healthcare sector, but within schools, local communities, and across business and industry). ‘COVID-19 may have created a new year-round baseline for work absences similar to flu season conditions before the pandemic’ - and those in national and local government - and those leading our NHS, schools, businesses and industry - should consider expanding protective interventions, for staff and their communities. And data collection, and monitoring, need to be ramped up to address the negative impacts of COVID-19 on the labour force - and on our local communities.
The elephant is still in the room, where those in leadership positions continue to ignore the simple, basic, scientific fact.
The SARSCoV2 virus is airborne, it always has been airborne, and it will continue to be airborne - as will its brothers and sisters, and its sons and daughters.
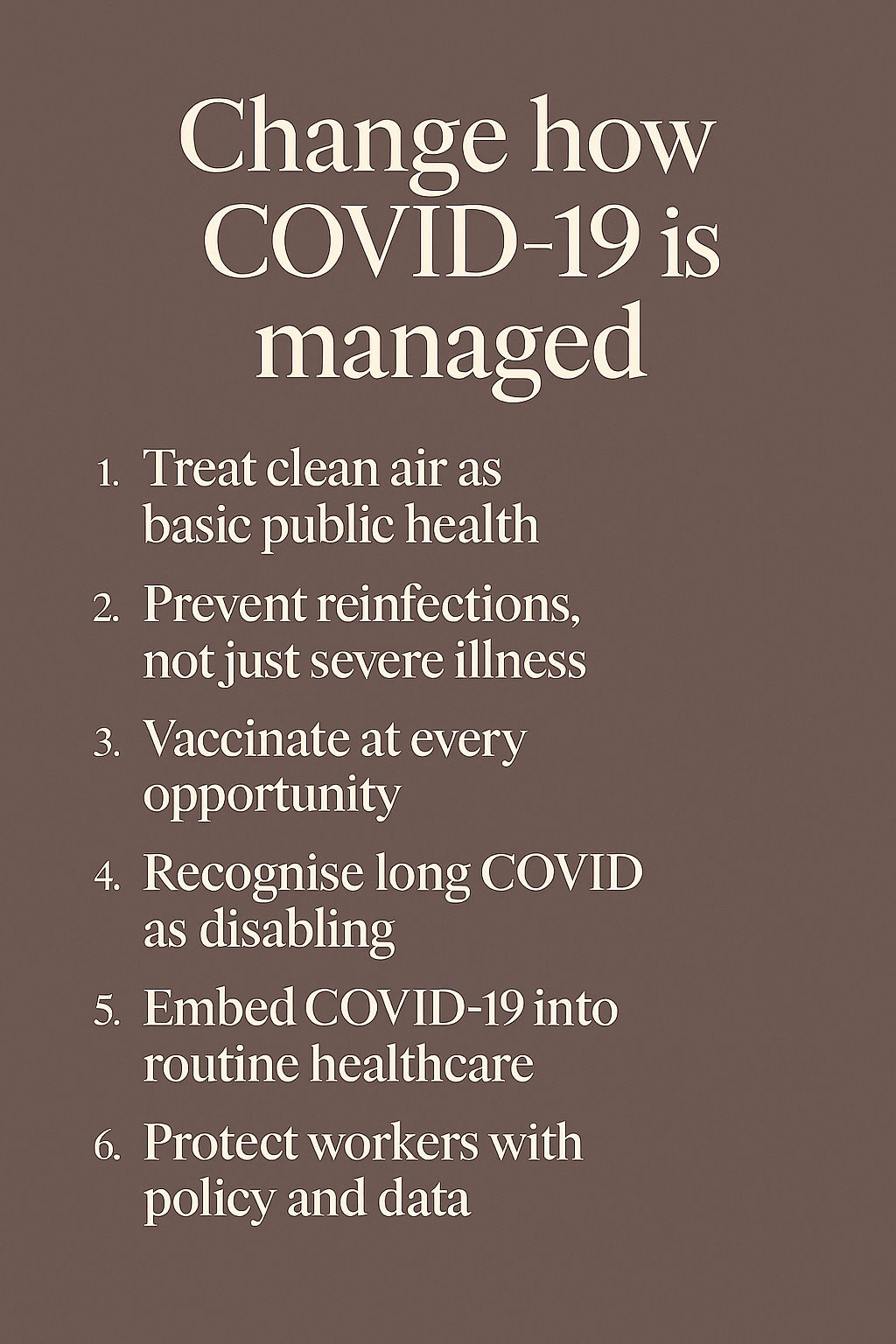
🧭 What needs to be done differently to manage COVID-19?
There needs to be a major shift from reactive crisis response to sustained, integrated strategies - centered on clean air, reinfection prevention, long COVID recognition, and resilient health systems.
1. Recognise, communicate, and manage airborne transmission as the prime mode of spread
Embed ventilation, filtration, and CO₂ monitoring into building design and building health and safety codes, workplace safety, and public health guidance.
Recognize clean air as a public health right - on par with clean water.
2. Prevent reinfection, not just severe illness
Reinfections increase the risk of Long COVID, organ damage, and workforce disability.
Shift the policy focus from hospitalisation to infection prevention, and control, especially in healthcare, schools, universities, on public transport, and in the world of work in general.
3. Long COVID - recognize, research, and respond to this significant challenge to the lives of those affected
Long COVID affects many millions of people globally - why do governments avoid monitoring and reporting the numbers - regardless of the challenges this presents?
Long COVID requires:
Effective central and local monitoring, recording, reporting, responding to the healthcare needs, and communications about Long COVID.
Dedicated clinics and research
Workplace accommodations
Inclusion in disability and workforce planning
4. Embed COVID-19 into routine healthcare systems
Globally, nationally and locally, there need to be a focus on integrating COVID-19 into respiratory disease programmes, primary care, and surveillance systems.
COVID-19 needs to be treated as a long-term public health challenge, not a temporary emergency.
5. Strengthen public healthcare infrastructure
Restore local public health capacity, increase staffing and training, and ensure early deployment of protective measures.
6. Improve workplace health and safety - and policy
The UK’s 2025 workforce strategy - specifically the ‘Keep Britain Working’ review -appears to have ignored COVID and Long COVID - and the need to revise infection prevention and control policy - and practice. Nationally and locally, the approach appears to be inconsistent and uncoordinated, often relying on limited understanding of COVID, Long COVID, and effective mitigation - worryingly, even within the NHS. Many healthcare professionals lack appropriate training, and some appear to dismiss the disease’s impact entirely. Worse still, there is widespread misunderstanding of airborne transmission, the importance of ventilation, and the benefits of vaccination.
Employers should:
Implement clean-air standards -and put these into action
Offer flexible return-to-work pathways
Track and report infection and post-infection impacts
7. Sustain and expand vaccination
The government and NHS should:
Maintain the highest possible coverage of updated vaccines.
Support and encourage global equity in vaccine access.
Integrate COVID-19 vaccination into routine immunisation schedules and annual campaigns.
In essence, comprehensive access to free COVID-19 vaccines is not merely a public health necessity but also a moral imperative. Ensuring every person, irrespective of their financial status, can receive the vaccine should be the ethical duty of our government. Failure to do so disregards the essential right to health care and the protection of our community.
To address this urgent issue, policymakers should allocate the necessary resources to the NHS, to enable them to distribute the COVID-19 vaccine universally and free of charge to all UK residents - regardless of age, but subject to guidance from their GP in relation to their own individual health context.
🔁 Summary: A New Public Health Model
There should a well-communicated recognition that COVID-19 is not over - it’s evolving. Managing its spread and impact now requires:
Clean air, and effective ventilation, as a public health right
Reinfection prevention as policy
Long COVID recognition as a disability issue
Integrated care, not emergency response
Workplace protections and data transparency
Vaccination as a sustained, equitable strategy


5 years on from contracting COVID, medical scientist Rebecca Broni is still living with its effects. @news.rte.ie
🛑She's not alone, though at times it must feel that way.
🦠This disease has affected many millions globally.
🤷Credible data doesn't exist.
💯Long COVID does!
https://www.rte.ie/news/2025/1128/1546309-long-covid-ireland/
💨Quote: @ukcovid-19inquiry.bsky.social 'is considering airborne transmission (and methods used to combat it) in the context of healthcare in Module 3: Impact of the Covid-19 pandemic on healthcare systems in the four nations of the UK'.
🤷It's STILL airborne!
https://covid19.public-inquiry.uk/reports/modules-2-2a-2b-2c-core-decision-making-and-political-governance-volume-i/